Diabetes ranks as one of the most prevalent chronic conditions worldwide, impacting millions across age groups. Healthcare providers must understand the complexities of diabetes management to provide effective care and improve outcomes. By diagnosing and monitoring blood glucose levels, managing lifestyle changes, and implementing pharmacological interventions, a comprehensive approach is essential. This course equips healthcare professionals with the latest strategies for diagnosing, managing, and preventing diabetes, enabling them to deliver compassionate, evidence-based care. Whether you’re a nurse, physician, or other healthcare provider, this training enhances your skills in addressing the challenges diabetes presents, fostering better health outcomes.
What You Will Learn:
- Risk factors for developing diabetes and prediabetes
- Principles of diabetes management, including medication, nutrition, and physical activity
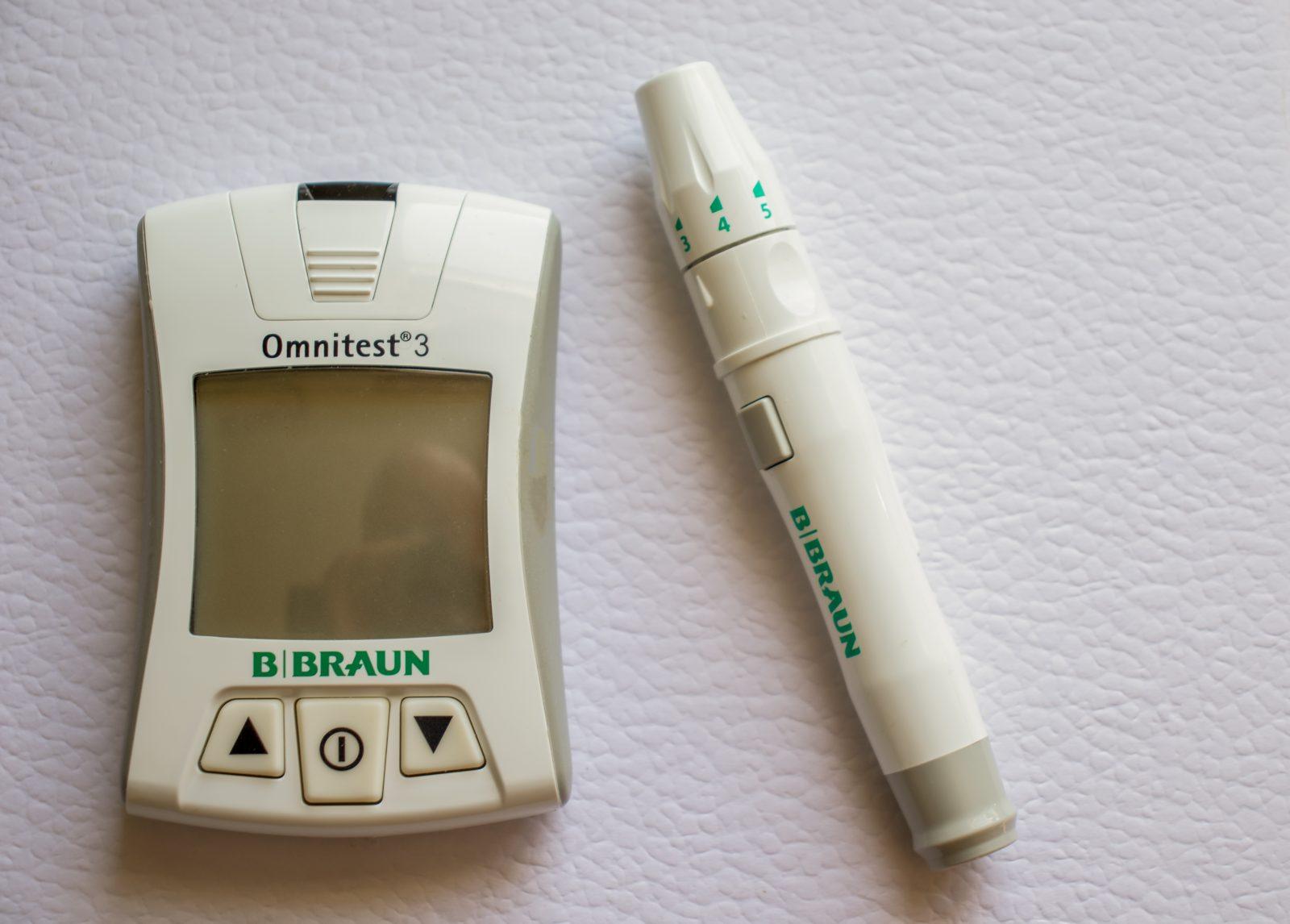
- Proper techniques for blood glucose monitoring and interpreting results
- Common acute and chronic conditions of diabetes, such as hypoglycemia, hyperglycemia, neuropathy, nephropathy, and retinopathy
- Effective patient education on diabetes self-management, including carbohydrate counting and meal planning
- The psychosocial impact of diabetes on patients and their families
Details:
Course length: 1 hour and 45 minutes; CME: 1.75
Languages: American English
Key features: Audio narration, learning activity, and post-assessment.
Get Certified
American Medical Compliance (AMC) is a leader in the industry for compliance, Billing, and HR solutions. To become certified, please visit us at: American Medical Compliance (AMC).
Reach out for other courses by visiting the AMC Course Library.
What is Diabetes?
Diabetes is a chronic condition where the body is unable to properly regulate blood sugar (glucose) levels. Glucose is the primary source of energy for cells, and its regulation is crucial for maintaining overall health. Insulin plays a vital role in helping glucose enter the bloodstream. In diabetes, the body either does not produce enough insulin or is unable to use it effectively, leading to high levels of glucose in the blood.
There are two main types of diabetes:
- Type 1 Diabetes: This type occurs when the immune system mistakenly attacks insulin-producing cells in the pancreas. It typically requires lifelong insulin therapy.
- Type 2 Diabetes: The body becomes resistant to insulin or the pancreas is unable to produce sufficient insulin. It is often linked to lifestyle factors such as poor diet, lack of physical activity, and obesity. Healthcare providers can manage Type 2 diabetes through lifestyle changes, medications, and in some cases, insulin.
Healthcare providers must understand the causes, symptoms, and long-term effects of diabetes to properly diagnose and manage the condition, improving the quality of life for individuals affected by it.
Maternally Inherited Diabetes Mellitus and Deafness (MIDD)
Maternally Inherited Diabetes Mellitus and Deafness (MIDD) is a rare mitochondrial disorder that is characterized by the combination of diabetes and progressive sensorineural hearing loss. Unlike most genetic conditions inherited through nuclear DNA, MIDD is linked to mutations in the mitochondrial DNA. Mitochondrial DNA is unique in that it is inherited exclusively from the mother, as the sperm lacks mitochondrial DNA. This pattern of inheritance explains why over 50% of individuals with MIDD have a mother who also has diabetes.
In individuals with MIDD, the mitochondrial dysfunction impairs insulin secretion, which results in diabetes. The associated hearing loss worsens over time, leading to sensorineural hearing impairment that may vary in sensitivity. As a progressive condition, MIDD can impact quality of life, requiring careful management of both diabetes and hearing loss.
Healthcare providers must understand MIDD to offer early diagnosis and effective management. Through genetic counseling and tailored treatment plans, healthcare providers can help manage symptoms and improve the quality of life for those with this condition.
Type 1 Diabetes: Causes and Risk Factors
Type 1 diabetes occurs when the body mistakenly attacks its own insulin-producing cells in the pancreas, resulting in the inability to produce insulin, which is crucial for regulating blood glucose levels. Unlike Type 2 diabetes, which is strongly influenced by lifestyles factors, the risk for Type 1 diabetes are not as well understood and are not clearly linked to preventable behaviors.
Although the exact cause is unclear, several known risk factors include:
- Genetics: A family history of Type 1 diabetes increases the likelihood of developing the condition. Specific genetic markers often appear in individuals with Type 1 diabetes, though not everyone with these markers will develop the disease.
- Autoimmune Response: An individual’s immune system may mistakenly destroy the beta cells in the pancreas. Infections or environmental influences are thought to trigger this autoimmune response.
- Age: Type 1 diabetes is most commonly diagnosed in children and young adults, though it can occur at any age.
- Environmental Factors: Certain viral infections or other environmental factors may trigger the autoimmune response in genetically predisposed individuals, leading to the onset of Type 1 diabetes.
Understanding these risk factors is important for early detection and management.
Symptoms of Diabetes: When to See a Doctor
If you experience any of the following symptoms, it may indicate that you have diabetes, and you should consult your doctor about getting your blood sugar tested:
- Frequent urination: Excessive urination, especially at night, may indicate your kidneys are working overtime to remove excess glucose from the blood.
- Increased thirst: Feeling constantly thirsty, even after drinking fluids, can result from your body trying to compensate for fluid lost through frequent urination.
- Extreme hunger: Despite eating, you may feel unusually hungry due to the body’s inability to properly use glucose for energy.
- Fatigue: Feeling unusually tired or weak, even after rest, can signal that your body is not effectively converting food into energy.
- Blurred vision: High blood sugar can alter the shape and flexibility of the lens in the eye, resulting in blurred vision.
- Slow-healing sores or frequent infections: High blood sugar impairs the body’s ability to heal and fight infections.
- Unexplained weight loss: Losing weight without trying, despite eating more, can occur when the body breaks down muscle and fat for energy due to insufficient insulin.
- Tingling or numbness in hands or feet: Prolonged high blood sugar can cause nerve damage, leading to tingling or numbness, particularly in the extremities.
If you notice any of these symptoms, it’s important to see a healthcare provider for a blood sugar test. Early detection and management of diabetes can help prevent complications and improve long-term health outcomes.
What is Continuous Glucose Monitoring?
Continuous Glucose Monitoring (CGM) tracks glucose levels throughout the day and night using a small sensor placed under the skin. This sensor measures glucose in the interstitial fluid and sends data to a device that provides real-time readings. Unlike traditional fingerstick tests, which provide a snapshot of glucose at a specific moment, CGM provides continuous, dynamic data.
CGM systems typically consists of three key components:
- Sensor: A small sensor inserted just under the skin that measures glucose levels continuously.
- Transmitter: Sends the glucose readings to a receiver or mobile app.
- Receiver or Display Device: Displays the glucose levels and trends, alerting the user to high or low glucose levels.
CGM helps people with diabetes, especially those using insulin, better manage their condition by providing detailed glucose trends. This enables more informed decision-making regarding insulin dosages, diet, and exercise. Some CGM systems also send alerts when glucose levels are too high or too low, helping individuals maintain more stable blood sugar levels.