Since the COVID-19 pandemic, health organizations have placed a greater priority in implementing proper infection control protocols, such as identifying cases of infections and supplying proper personal protective equipment (PPE) to emergency medical workers. All medical facilities must establish and follow proper infection control guidelines due to the high potential of exposure to infectious materials and patients that healthcare personnel face.
Emergency medical workers also must implement and follow an infection control plan.
Moreover, the following Infection Control Training for Emergency Medical Services (EMS) educates emergency medical workers on how to protect themselves and their patients while mitigating community transmissions of infectious diseases. Emergency medical workers will learn about infection control procedures, recommendations for patients, how to evaluate and test persons suspected of infection, and methods for controlling exposure.
What you’ll learn
- Recommendations for minimizing chances of exposure
- How to care for patients with suspected or confirmed COVID-19 infection
- Preparations that need to be made for infectious patient arrivals
- Methods of evaluating and testing persons suspected of COVID-19 infection
- Protective measures to control exposure
Details
Course length: 30 minutes; CEU: 0.5.
Languages: American English
Key features: Audio narration, learning activity, and post-assessment
Get Certified
American Medical Compliance (AMC) is a leader in the industry for compliance, Billing and HR solutions. To become certified, please visit us at American Medical Compliance (AMC).
Reach out for other courses by visiting the AMC Course Library.
Infection Control Procedures for Emergency Medical Workers
Emergency medical facilities must implement put policies and practices in place to help minimize exposures to respiratory pathogens, such as SARS-CoV-2, the virus that causes COVID-19. Emergency medical workers should implement these measures before patient arrival, upon arrival, during the patient’s visit, and until the patient’s room has been fully cleaned and disinfected.
Facilities can implement these measures in several ways. For example, emergency medical workers use triage protocols to assess patients suffering from respiratory infections. Additionally, workers can limit points of entry to the emergency medical facility.
Infection Control Procedures When Caring for Patients with COVID-19 Infection
It is important for emergency medical workers to have infection control procedures in place prior to encountering a patient with confirmed or suspected COVID-19. Emergency medical workers face an increased risk of exposure to COVID-19.
This training provides recommendations for emergency medical workers on minimizing the risk of exposure when caring for confirmed or suspected COVID-19 patients. This course begins with an in-depth explanation of COVID-19 transmission. Due to the fact that COVID-19 is a fairly new disease, there is still uncertainty within the healthcare field about its transmission.
How to Prepare for a Patient with an Infectious Disease
Emergency medical workers must transport and give care to patients with confirmed or suspected COVID-19 in line with infection control guidelines. They should be familiar with the symptoms of COVID-19 so that they can properly evaluate patients. This course highlights key steps that emergency medical workers can take in preparation for transporting and providing care to patients with confirmed or suspected COVID-19. For example, emergency medical workers should review their infection prevention policies in alignment with CDC infection control recommendations. This includes assessing patients with respiratory symptoms, placing patients in rooms, proper use of PPE, and visitor restrictions.
Evaluating and Testing Persons Suspected of COVID-19 Infection
There is a proper protocol to follow for reporting a person for a suspected case of COVID-19 infection. It is crucial to identify persons suspected of COVID-19 infection and give them proper testing to limit the spread of SARS-CoV-2. This course discusses some approaches to reporting persons suspected of COVID-19 infection validated by the CDC. The CDC uses COVID-19 testing data to track the impact of the outbreak and inform a reasonable public health response. The CDC collects data such as demographic and clinical characteristics, exposure and contact history, and course of clinical illness and care received from persons confirmed to have COVID-19 to better understand the epidemiology of COVID-19. In this course, we also offer tips on submitting this data to the CDC.
If you are concerned that a patient may have COVID-19, please report this information to your manager or supervisor immediately. The CDC is working in partnership with state and local health departments to support those confirmed to have COVID-19. For more information, please contact your state or local health department.
Limiting Exposure Through Infection Control Procedures
Controlling exposures to occupational hazards is a fundamental way to protect emergency medical workers. Typically, a hierarchy of controls is used to feasibly and effectively implement infection control measures. Multiple infection control strategies can be implemented concurrently and/or sequentially.
In this course, we go into specific detail about each aspect of the hierarchy of controls.
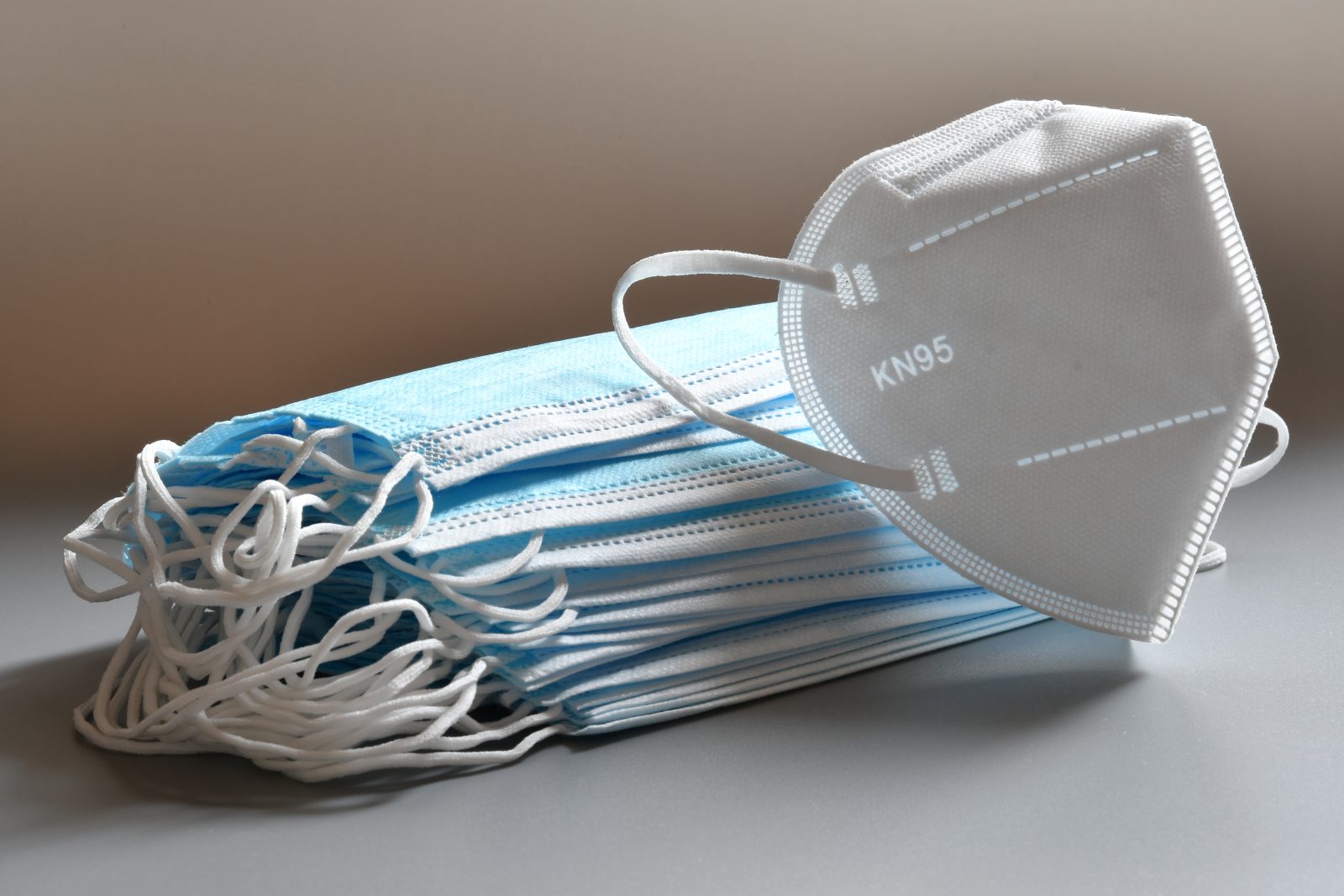
Safe use of Personal Protective Equipment (PPE) for Emergency Medical Workers
This course describes the proper sequence for putting on or donning personal protective equipment (PPE). The type of PPE used will vary based on the level of precautions required. The procedure for putting on and removing PPE should be tailored to the specific type of PPE.
It is crucial for emergency medical workers to properly put on personal protective equipment to be fully protected from infectious diseases. Further, there are certain recommendations on preferred types of PPE versus others, which this course discusses at length.
The World Health Organization has specifically emphasized the importance of respirators in preventing COVID-19 transmission.
Emergency Medical Facility COVID-19 Infection Control Policies
The true extent of the COVID-19 outbreak within our community cannot be predicted. However, all emergency medical facilities can take steps now to prepare for future outbreak and protect patients and staff. It is crucial to be prepared!
Emergency medical facilities need to stay informed about the COVID-19 situation specific to their community. The CDC and state and local health departments are sources of reliable, up-to-date information regarding COVID-19. If you have not already developed an emergency plan for your facility, do so now.
If you already have an emergency plan in your facility, it may be necessary to review it. Being prepared for situations like increased transmission or staff absenteeism will be essential to the functioning of your emergency medical facility.
Additional Infection Control Recommendations for Outpatient Facilities
Outpatient dialysis facilities should have established policies and practices to reduce the spread of contagious respiratory pathogens. This course provides guidance for outpatient dialysis facilities based on currently availably COVID-19 information. It is important to note that recommended actions may be subject to change as more information becomes available
This Infection Control Training for Emergency Medical Services (EMS) can be done online at your own pace. Training materials can be accessed using any device. An online training course also enables you to receive training regardless of location for as long as you can access the net.